The rise in Mpox cases beyond its usual regions in Africa, reaching as far as Sweden and California, has cast a harsh spotlight on the vulnerabilities in global disease prevention systems.
Despite existing awareness and prior outbreaks, the rapid and unexpected transmission of this virus, formerly known as Monkeypox, has exposed the limitations and challenges faced by leading health organizations like the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC).
According to CNN, “The Africa Centres for Disease Control and Prevention declared the outbreak a public health emergency of continental security on Tuesday, the first such declaration by the agency since its inception in 2017.”
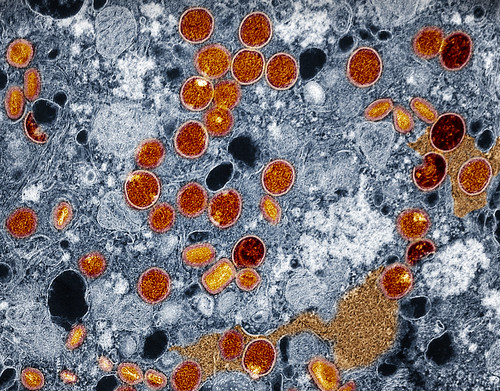
Mpox was first identified in humans in the 1970s and has been managed before. Historically, outbreaks were mostly limited to central and western Africa and spread primarily through contact with infected animals.
In an interview with The Hilltop, Howard University College of Medicine professor Dr. Karl Thompson discussed the characteristic symptoms of monkeypox.
“Monkeypox is characterized by painful circular rashes on the skin with additional inflammatory symptoms such as fever, headache, muscle aches, and fatigue,” Dr. Thompson said. “Monkeypox is related to smallpox, an older infectious disease that was eradicated through widespread vaccination.”
However, the virus has spread into urban settings and across continents. The recent outbreak in the U.S., with cases in California, marks a significant shift in the virus’s trajectory. This raised critical questions about how global health defenses missed it.
In the same article, WHO Director-General Tedros Adhanom Ghebreyesus emphasized the necessity of a unified global approach.
“It’s clear that a coordinated international response is essential to stop these outbreaks and save lives,” he said.
Dr. Thompson also highlighted the implications of the outbreak and how it could impact the Howard community.
“Given that we have an international population in the USA, the District of Columbia, as well as Howard University, this is something that we should keep an eye on,” he said.
The call for international cooperation highlights the interconnected nature of modern public health challenges where a disease in one part of the world can quickly become a global threat.
What’s missing?
Below are some potential gaps that may have occurred in the global disease prevention framework:
1. Delayed Detection and Response:
Initial cases in unusual countries could have either been misdiagnosed or not immediately reported, which may have allowed the virus to spread unchecked. For instance, the lack of awareness about monkeypox symptoms among healthcare providers in regions where the disease is not common. The delays in immediate containment points to the need for more proactive and robust disease monitoring.
2. Global Coordination Challenges:
Inconsistent and delayed responses between countries have created challenges. Without seamless communication and collaboration, efforts to control the spread of diseases like monkeypox can become disjointed and lead to a higher risk of transmission.
3. Limited Vaccine Deployment:
While Mpox vaccines exist, they are not widely available, which may have limited outbreak containment. Global vaccine distribution challenges, similar to those during the COVID-19 pandemic, highlight the fragility of global health systems, especially in low-resource settings.
Tedros said that vaccines are only part of the response. Containing the spread will also require increased surveillance, diagnostics and research to fill “gaps in understanding.”
Health organizations must prioritize strengthening early warning systems, fostering better international collaboration and investing in research and development for vaccines and treatments for emerging infectious diseases.
As the modern world faces an increasing number of emerging infectious diseases, it is important now more than ever to develop a resilient, coordinated and proactive approach to disease prevention and control.
Copy edited by Anijah Franklin